Conference Reflections
In June 2025, thousands of psychiatrists, researchers, and clinicians met in Wales for the Royal College of Psychiatrists International Congress 2025. This is one of the UK’s leading conferences in mental health, exploring emerging challenges, scientific advances, and human experiences at the heart of psychiatry. I was particularly drawn to sessions on insomnia, neurodevelopmental conditions, intergenerational mental health, and the therapeutic value of storytelling in forced migration. I share some of my reflections and takeaways from the conference here.
The Insomnia Epidemic
- Dr Lauren Waterman highlighted the complexity of managing chronic insomnia, especially when layered with other conditions like chronic fatigue or substance use. She advocated a stepped care approach, noting that CBT for insomnia (CBT-I) might not always be enough, particularly in chronic cases where medication may be necessary. She noted that waking up in the nighttime is actually normal and evolutionarily developed as a survival technique, however it is the worrying about waking up in the night time which contributes to insomnia.
- Dr Rajiv Shah built on the mechanics of CBT-I, emphasising conditioned hyperarousal, where the bed becomes associated with wakefulness rather than sleep. Common habits, such as watching TV or working in bed, unintentionally reinforce insomnia by associating a place of restfulness with stimulation. His strategies include stimulus control, a 15-minute rule (leave the bedroom if you can’t sleep within 15 minutes), and consistent anchor wake times to train the body into following a particular sleep schedule. These not only improve sleep efficiency but also help restore confidence in natural sleep, especially when supported by behavioural and cognitive strategies like paradoxical intent and imagery techniques.
- Dr Jacob King outlined how CBT-I can be adapted for mental health and addiction services, particularly when sleep disturbances intersect with alcohol dependence, PTSD, and depression. He described the Westminster Sleep Group’s six-week programme, which combines psychoeducation, diary tracking, and environmental adjustments. He called for flexibility in sleep interventions, recognising contextual challenges such as shift work, sofa surfing, and environmental noise, which reflects how sustainable sleep is often rooted in social justice as much as clinical technique.
- Overall, this session emphasised how there is a high prevalence of insomnia globally and that treating insomnia directly benefits the physical and mental health of patients.
Autism and ADHD
- This session covered the theme of evolving diagnoses for generalist psychiatrists for autism and ADHD. Dr Quinton Deeley laid out the changing landscape of autism and ADHD over the past few decades, reinforcing that autism should be seen as a condition, not a disorder. He emphasised the positive attributes like attention to detail, strong memory, and originality. He discussed blurred lines between autism and ADHD, such as with executive dysfunction, emotional dysregulation, and inattention.
- Autism has historically been labelled as childhood psychosis, and is now understood to be part of neurodiversity. Dr Deeley called for better recognition of autism in women and those with complex presentations. Clinically, he emphasised social support, employment assistance, and treating co-occurring conditions, including low-dose antipsychotics for anxiety when needed, as important steps forward.
Art and Science of Mental Health
- This provided an overview of examples of preventative interventions on post-partum serious mental illness, psychosis, adolescent mental health, early intervention in psychosis, multi-morbidity, and preventive policies for mental health.
- The interventions include digital and in person approaches, population and individual level.
- The session was interdisciplinary, including researchers and clinicians, using data and statistical insights to highlight the importance of focusing on mental health. This session was delivered in partnership with the Public Mental Health Implementation Centre (PMHIC).
Intergenerational Transmission of Mental Health Conditions
- Researchers explored how parents’ mental health affects their children, and what interventions might prevent transmission. Dr Abigail Dunn presented on the “Raising Confident Children” course, a digital programme aimed at parents with anxiety disorders. By focusing on parenting skills (e.g., emotion coaching, limit setting, managing overprotection), rather than the child’s anxiety, it showed promising public health impact and scalability.
- Professor Steve Jones brought attention to parents living with bipolar disorder, sharing insights from the IBPI study and underscoring the urgent need for accessible, digital support tools. While many children of parents with bipolar face their own mental health risks, services often only respond after conditions are well-established. The emphasis was on early, preventive, family-centred interventions.
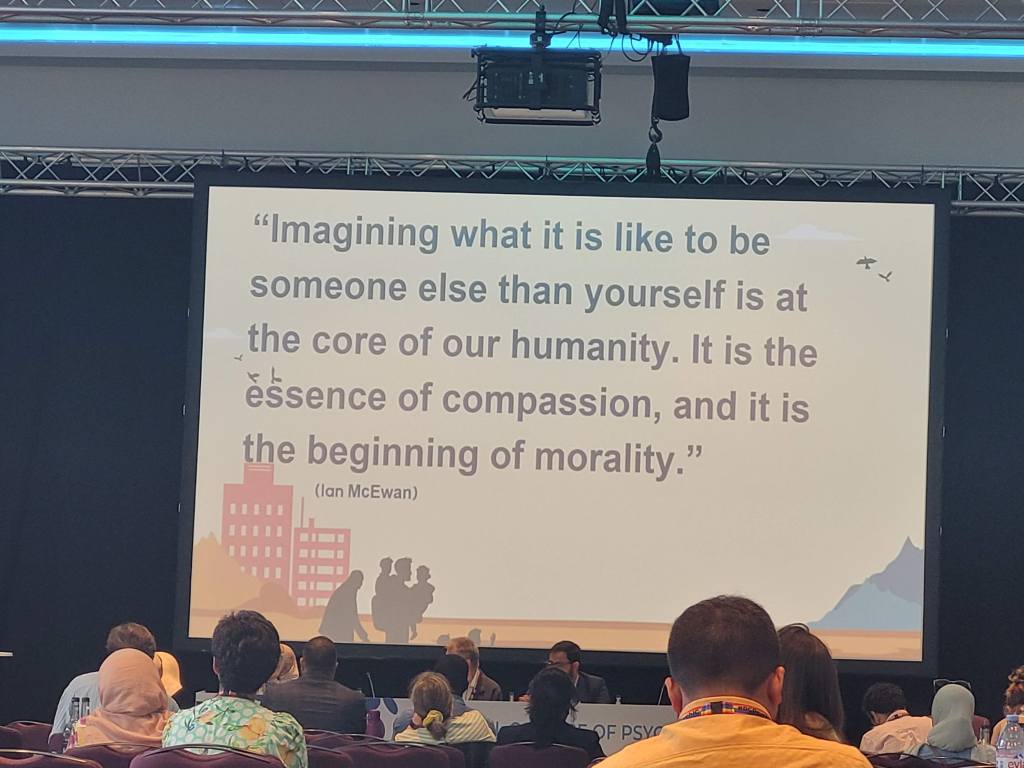
Forced Migration and Mental Health
- This session highlighted the role of narratives and empathy in understanding the trauma associated with forced migration. It brought together an interdisciplinary approach across the arts, literature, lived experience, and clinical psychiatry.
- Professor Femi Oyebode used classical texts like the Iliad to illustrate enduring psychological impacts of displacement. Mr Gulwali Passarlay shared his own refugee story, underlining that the journey through asylum systems can often be more mentally taxing than the physical migration itself. He talked about his book, The Lightless Sky, where he shared his journey.
- Dr Yasir Hameed explored how films such as His House, Human Flow, and Limbo can educate clinicians on compassion fatigue and the cultural context of trauma. Professor Cornelius Katona highlighted the challenges of bearing witness to fragmented and evolving stories in clinical practice. Storytelling, he argued, is both therapeutic and diagnostic, and must be treated with care.
Advances in Precision Psychiatry
- Professor Naomi Fineberg highlighted new research into precision psychiatry, showing how key traits like cognitive inflexibility, impulsivity, and habitual behaviours present in OCD. She showed findings showing deep brain stimulation improving cognitive flexibility in treatment-resistant cases. With high relapse rates and undiagnosed comorbidities like autism in up to 50% of OCD patients, the case was made for precision psychiatry, targeting underlying cognitive profiles rather than surface behaviours alone.
This year’s congress highlighted how psychiatry is a multidisciplinary specialism, across the clinical sciences, arts, and humanities. It emphasised the human side and story to psychiatry, and why it’s important to be culturally and contextually sensitive.
I am grateful to the Royal College of Psychiatrists for their support and for the award to attend this prestigious conference and learn from the UK’s leaders in the field of mental health.